Viewing men as the default human has been human society. This habit is deeply set, from language – where the word “man” stands for both men and the entire species – to healthcare, where medical education has focused on a “male” norm that assumes the male body is representative of the human body. This male-centric thinking has left a “female shaped” gap in human history– the gender data gap – and its impact can be felt in women’s lives every day.
In a world where humanity is becoming increasingly reliant on data, the impact of the gender data gaps will be even greater. If the data we use is corrupted by gaps, the information we are trying to uncover will always be flawed, especially for women.
But how is the gender data gap affecting health care?
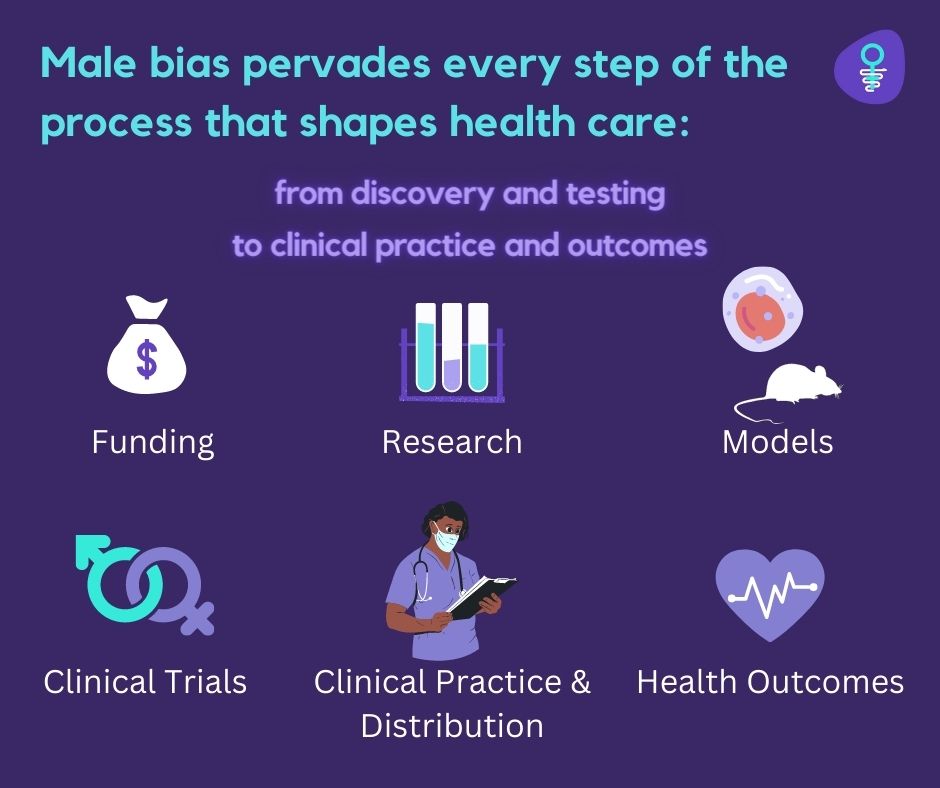
Gender data gaps can be found every step of the process that shapes health care: from discovery and testing to clinical practice to outcomes.
- Females are often excluded or underrepresented in the cells, animals, and humans studied in biomedical, clinical, and public health research. Only 30%, 43%, and 54% of the 11.5 million papers published between 1980 and 2016 reported on both male and female populations.
- Even when females are included in studies, researchers rarely analyze or report results by sex (biological characteristics) or gender (societal norms and behavior).
- Clinical guidelines and practice often ignore sex and gender differences, using men as proxies for women.
- When measuring effectiveness, it is again not the norm to disaggregate outcomes for women.
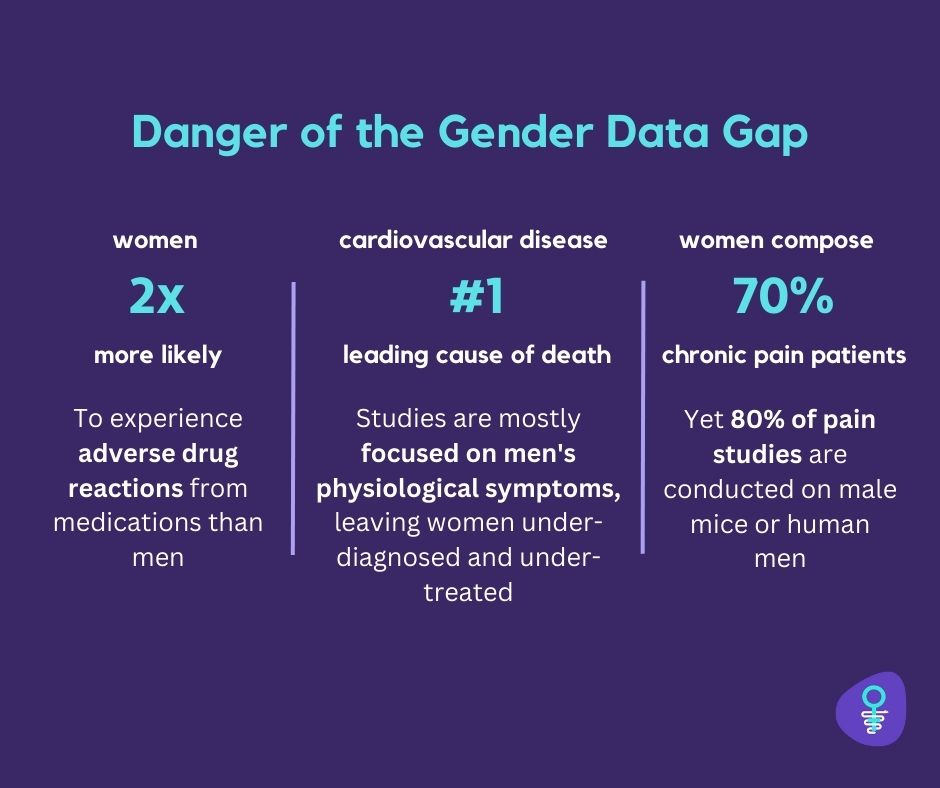
Unsurprisingly, the lack of information about women’s health is putting women’s lives at risk in countless ways. This includes care delays and errors, adverse drug reactions, and lower survival rates in certain diseases.
Care delays and error
Doctors tend to misdiagnose, underdiagnose, or undertreat diseases that predominantly affect women, or in situations where women present with different symptoms for common diseases, because men are seen as the default human. For example, heart attacks are more likely to be misdiagnosed in women because they don’t always experience the typical (male) symptom of chest pain.
Adverse drug reactions
As previously described, women are often excluded or underrepresented in health research. This has led to more adverse effects, with women’s risk being 1.5-1.7 times higher than that of men. One of the risks is that the standard (male) dose may be too high for women. To illustrate this: Eight out of 10 prescription drugs taken off the market between 1997 and 2001 were more dangerous for women.
Lower survival rates:
Women have different heart disease (among others) which is the leading cause of death globally for both sexes. In the United States, more women than men die within a year of a heart attack (26% versus 19%, respectively). This pattern persists within five years (47% versus 36%), perhaps because women are less likely to receive a correct diagnosis or be prescribed medications to lower their risk of heart attacks.
What risks does the newfound significance of data pose to women’s health?
Algorithms have the potential to amplify historical biases, including those based on gender and race, which can put female patients at risk of misdiagnosis and poorer outcomes. For instance, an algorithm trained on male-biased data to recognize “typical” heart attack symptoms could misdiagnose many women. Physicians and patients may then assume that algorithms are unbiased and infallible, which can lead them to ignore contradictory information and result in automation bias. This makes it harder to prevent or detect mistakes, which can further erode the trust of women who already struggle to get accurate diagnoses and effective treatments.
Who is looking to close the gender data gap?
Let’s take a look at a few key players that are actively working to close the gender data gap.
- Women at the Table is a global civil society organization based in Geneva, Switzerland. Their goal is to expose the systematic exclusion of women from defining rules and to identify strategic changes to laws, regulations, and norms.
- theblood is a FemTech company based in Berlin, that developed a new approach to blood analysis using menstrual blood helping people access, understand, and benefit from unprecedented data.
- DotLab is a women’s healthcare technology company that aims to improve the diagnosis of active endometriosis by developing a blood test called that measures specific biomarkers.
- Dama Health aims to advance the field of contraception fit. By taking into account a user’s preferences, medical history, and previous experience, their technology finds the most suitable type and brand of contraception.
