The following is an interview about Vulvodynia by Francesca Rosa with Silvia Carabelli, Political activist and co-founder of the Italian Committee for vulvodynia and pudendal neuropathy and Dr. Med. Chiara Marra, Specialist Doctor in Gynecology and Obstetrics, health director of the clinic CasaMedica and co-founder of the Italian Committee for vulvodynia and pudendal neuropathy.
Let’s set the stage: How many women does Vulvodynia impact and how many specialists are actually aware of this syndrome. Dr. Med. Marra – happy to have you here. Let’s start with you.
 Dr. Marra: 10-16% of women worldwide experience vulvodynia. Only 60% of women reporting chronic vulvar pain seek treatment, and only about half will receive a correct diagnosis.
Dr. Marra: 10-16% of women worldwide experience vulvodynia. Only 60% of women reporting chronic vulvar pain seek treatment, and only about half will receive a correct diagnosis.
45 to 65% of gynecologists lack diagnostic knowledge of vulvodynia. About 20% of gynecologists actually know about vulvodynia but don’t feel able to initiate treatment. Which leaves only 20% of gynecologists actually knowing about vulvodynia and feeling able to initiate appropriate treatment.
Dr. Marra: Vulvodynia consists of vulvar pain that lasts for more than 3 months without an identifiable cause. Due to the lack of an identifiable cause, this condition is often referred to as a diagnosis of exclusion. Despite its definition, in my view this disease is exactly like any other, even if it is not characterized by specific and clear symptoms at the vulvar level. Therefore, it would be better to talk about differential diagnosis, meaning that it should be considered on a par with the other vulvovaginal conditions during the examination process.
The vulvar pain occurs in different ways: in some women it manifests itself as itching, in others as burning, in others as a sensation of “pins” or “electric shocks”, in others as a real strong pain that can even affect walking. The pain can be spontaneous or triggered by tight clothing, intimate hygiene, touch, or sexual intercourse. The most common form of vulvodynia is the so-called “provoked vulvodynia”, which is clearly accompanied by a deterioration of sexual desire and intimacy.
Vulvodynia can be associated to several factors that, acting in a synergistic way, may trigger and subsequently maintain it. These include infectious factors (recurrent vaginitis and cystitis), pelvic floor dysfunction (hypercontractility of the muscles), hormonal factors (e.g., low estrogen levels such as those found when taking the contraceptive pill or during menopause), psychosocial factors (e.g., traumatic sexual experiences in the past), and peripheral and central mechanisms involved in the genesis and maintenance of pain.
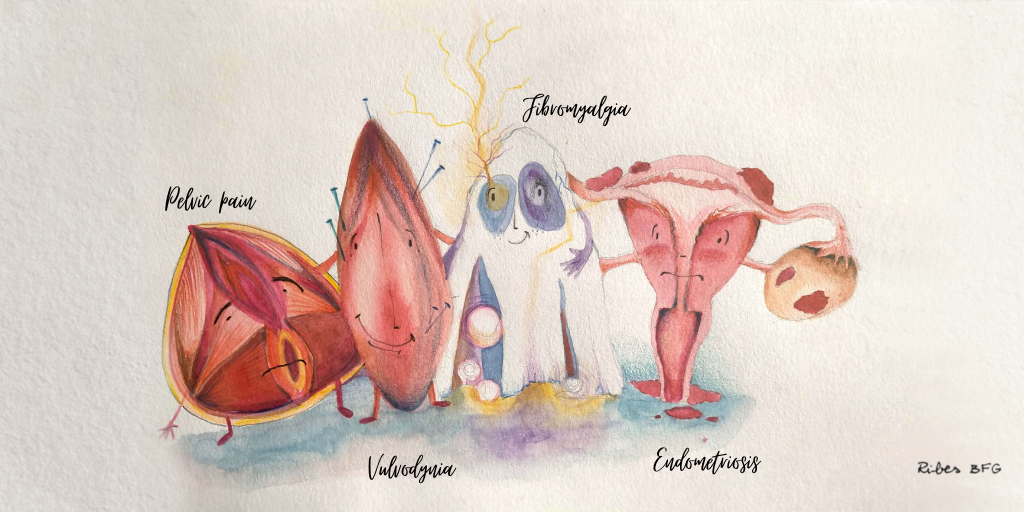
Pain is transmitted through nerves and may express itself both at the peripheral level (i.e., at the nerve endings in the genitals) and at level of the central nervous system. At the entrance of the vagina, the nerve endings are much more numerous and thickened in women with vulvodynia than in others, and therefore much more “receptive”. At the central level, vulvodynia is thought to be part of one of those central hypersensitization syndromes, such as fibromyalgia, chronic fatigue syndrome and irritable bowel syndrome, characterized by a dysregulation of endogenous pain modulation systems and persistent sensitization of neurons even after cessation of the stimulus that activated them.
 Okay Silvia, I have a few questions for you now. You’re a Political activist and co-founder of the Italian Committee for vulvodynia and pudendal neuropathy. Could you briefly speak to what the impact of vulvodynia is on a woman’s daily life?
Okay Silvia, I have a few questions for you now. You’re a Political activist and co-founder of the Italian Committee for vulvodynia and pudendal neuropathy. Could you briefly speak to what the impact of vulvodynia is on a woman’s daily life?
Silvia: Vulvodynia is defined as a dynamic disability because it is invisible. In most cases it compromises, partially or totally, the sexual life of women as it causes pain during sexual intercourse, also not-penetrative ones (e.g., when the disorder involves the clitoris in the form of clitoridodynia or clitoral hypersensitivity).
Additionally, depending on the severity of the disease, vulvodynia can affect other daily actions, such as peeing, sitting, wearing underwear, tights and tight pants, washing, going to the pool or the beach, doing sports, sometimes even walking.
Thanks to a correct and early diagnosis, the chronicity of the syndrome and the worsening of the symptoms could be avoided. An appropriate treatment and a multimodal approach can lead women to recovery or a partial remission of symptoms that allow them to live well with the disease.
Dr. Marra, back to you – Why has the condition not gotten much attention if it impacts up to 16% of the female population?
Dr. Marra: There are many reasons. Undoubtedly, the main reason is that pain felt by women is usually underestimated by the health care personnel, due to a cultural tendency to normalize menstrual pain, vulvovaginal discomfort and pain during intercourse. The second reason is that often symptoms are unconsciously minimized by specialists, to avoid feeling frustrated when they cannot find a clear explanation for them. Obviously, the correct attitude should be to study, get informed, gather information, but unfortunately this does not always happen.
On the other hand, the data tell us that only 60% of women talk to their doctor about the vulvar pain that afflicts them. This attitude also has a cultural background that is rooted in shame, in the endurance of pain, in always taking a back seat to the needs of the partner or the family. It has roots also in the inability to create a proper setting of dialogue and openness between doctor and patient during the gynecological visit.
Finally, vulvodynia is a complex pathology that must be managed in a multimodal way and that requires the knowledge of drugs for pain control that rarely a gynecologist or a urologist (the figures who most frequently treat it) know how to handle. Therefore, it requires specific training and a team approach (not always easily achievable, especially in the public health service).
Okay, last question, Silvia, how is the political landscape changing in regards to Vulvodynia and what still needs to be done?
Silvia: Vulvodynia was officially recognized by the World Health Organization (WHO) in the 11th revision of the International Classification of Diseases (ICD), which became effective on January 1, 2022.
Given my experience, I will now focus on Italy, whose health system is very different from that of Switzerland, due to the existence of the Sistema Sanitario Nazionale (publish health system, abbreviation: SSN). I will start with a brief overview on that. The Italian public health system is financed through tax funding and a partial participation in public spending by citizens with a medium-high income. This system was thought to guarantee the right to health and care for all human beings, including those who need free assistance, such as citizens in a state of severe indigence and immigrants without regular documents.
Chronic and disabling diseases often require a prolonged health care expenditure, sometimes even for life, and imply a certain degree of disability, which can cause the inability to work for people who suffer from them. Therefore, they are generally recognized in the Essential Levels of Care (Livelli Essenziali di Assistenza, abbreviation: LEA) by the SSN. The LEAs ensure free healthcare for such patients in the public system, providing free medical examinations, treatments, and drugs.
To date, however, vulvodynia is not recognized in the LEAs, despite being a chronic and disabling disease. This exclusion implies several problems:
- Absence of public clinics specialized in the diagnosis and treatment of the disease.
- Paid examinations and treatments in private clinics.
- Drugs paid for at full price, often prescribed for off-label use.
- Inability to apply for a disability pension based on the severity of the pathology.
The progress made in the Italian landscape is mainly due to four main drivers.
- The effort of associations, which for years have been raising awareness of the disease.
- The internet, including social networks, which is acting as a source of information and gathering for patients, who can> meet and support each other on the way of diagnosis and treatment.
- The action of some influencers who shared their personal experience on social networks and thus allowed many women and girls to self-diagnose this disease (to date, the diagnostic delay is still, on average, 4 years and a half).
- A further important contribution to the cause come from the recent establishment of the Comitato vulvodinia e neuropatia del pudendo (Committee vulvodynia and pudendal neuropathy). It brings together the 6 Italian associations that for over 15 years have been playing a crucial role for awareness-rising, the few health professionals specialized in the treatment of these diseases and several patients, who are also political activists. The aim of the Committee is to obtain the recognition of these diseases by the Italian State. Alongside the Committee, also the feminist movement Non Una Di Meno (Not one less) supports the path of recognition of this pathology, which affects the population assigned female at birth and that, to date, is still very underestimated and misunderstood.
In this scenario, much remains to be done:
- Obtain the recognition of vulvodynia in the LEAs, with all the rights that this entails.
- Obtain funds for scientific research to deepen the knowledge on this disease.
- Implement academic and practical training of health professionals who today, on average, do not know this disease.
- Establish pelvic units in public hospitals for the treatment of chronic pelvic pain because vulvodynia often occurs associated with (or is a consequence of) other diseases, such as endometriosis, irritable bowel syndrome, pudendal neuropathy, painful bladder syndrome and fibromyalgia. It therefore requires a holistic view of the patients and a multimodal treatment that acts on the various concomitant or comorbidities of the disease.
We wanted to close off this interview with a stat: Did you know that 2 in 5 women report having vaginal discomfort and painful sex? And yet, until recently, there haven’t been services or products on the market to address these issues. That’s why we need femtech (and a femtech summit like this one) to feature prominent solutions in the space. Want to read more about vulvodynia and how it’s gone ignored for far too long ? Check out this article : https://www.bbc.com/future/article/20180725-the-health-condition-vulvodynia-is-painful-and-misunderstood and don’t forget to sign up for the 2022 femtech conference here